| Intention Tremors
|
|
Cerebellar Ataxia. Cerebellar ataxia is a disorder in wihch the patient has difficulty in movement and balance and a failure to coordinate muscle movements. Cerebellar lesions give rise to an intention tremor: the coarse tremor increases as the limb attempts to reach the object of the desired voluntary movement. The intention tremor is usually at right angles to the direction of movement, and the hand alternates between overshooting and undershooting their target. Unilateral cerebellar lesions cause a loss of muscle tone on the same side as the lesion. Nystagmus and disturbances of the vestibulo-ocular reflexes may also be present. Cerebellar Ataxia is sometimes a feature of Multiple Sclerosis. |
Intention Tremor in the left arm of the patient, attempting to touch his right index finger |
|
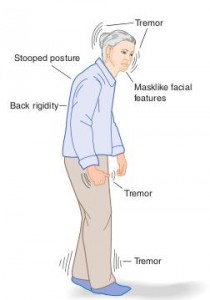
The French neurologist Jean-Martin Charcot identifide the difference between intention an non-intention tremors. He realised that patients with Parkinson's disease had a tremor at rest, and which disappeared during voluntary movements. In contrast there were a different group of patients with different signs and symptoms, including a tremor that only occurred during a voluntary movement and which prevented the limb reaching its desired destination, i.e. an intention tremor.. Charcot's triad is a group of symptoms and signs including an intention tremor, nystagmus and scanning speech. Many of these patients had Multiple sclerosis, but other had other forms of cerebellar disorder. | The most common cause of intention tremors is damage to the cerebellum. These patients have difficulty in executing movements, such as a probelm with attempting to touch their nose or another obejct with a finger (known as dysdiadokokinesis). Common sites for cerebellar lesions that lead to intention tremors include:
|

 *
*